- What is the IVF Process?
- Fertilization
- Embryo Development and Monitoring
- Challenges and Success Rates
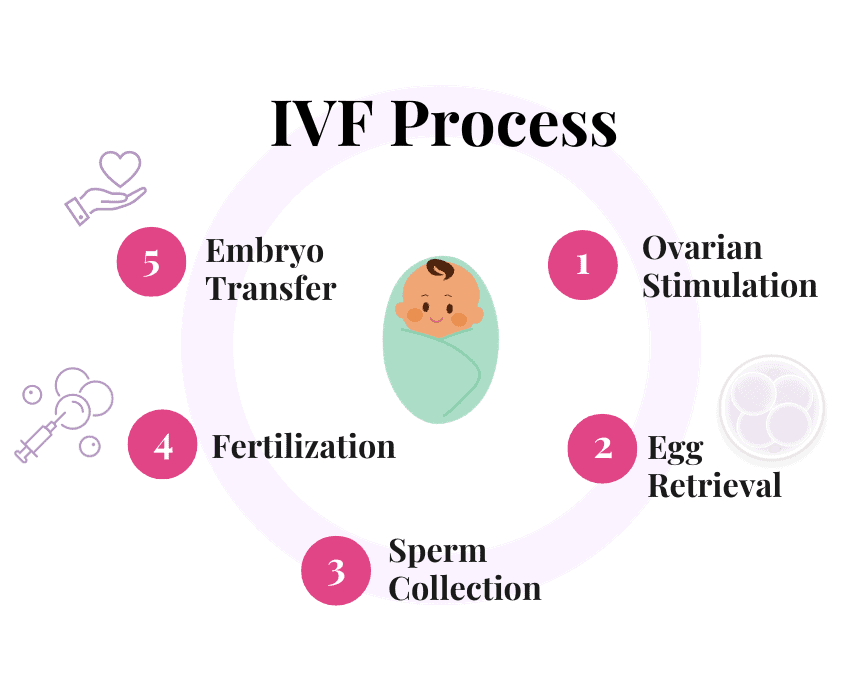
In vitro fertilization (IVF) is a widely known and commonly used assisted reproductive technology that helps individuals and couples overcome infertility and achieve pregnancy. “The IVF process involves fertilizing an egg with sperm outside the body in a laboratory setting, after which the resulting embryo is transferred to the uterus,” says Laurel Stadtmauer, M.D., Ph.D., a board-certified physician specializing in Endocrinology and Infertility at The IVF Center.
The IVF Center aims to provide an in-depth understanding of how IVF works, including the steps involved and the potential challenges and success rates associated with the procedure.
What is the IVF Process?
The first step in the IVF process is ovarian stimulation, which involves the administration of fertility medications to the woman to stimulate the ovaries to produce multiple mature eggs.
Typically, these medications are hormonal injections given over 8-14 days. Frequent monitoring through blood tests and ultrasound examinations is conducted to track the development of the ovarian follicles and adjust the medication dosage if necessary.
Egg Retrieval
 Once the ovarian follicles have reached the appropriate size and maturity, the eggs are retrieved in a minor surgical procedure known as transvaginal ultrasound-guided egg retrieval.
Once the ovarian follicles have reached the appropriate size and maturity, the eggs are retrieved in a minor surgical procedure known as transvaginal ultrasound-guided egg retrieval.
The woman is usually placed under mild anesthesia, and a thin needle is inserted through the vaginal wall into each follicle to aspirate the fluid containing the eggs. The retrieved eggs are then immediately transferred to the laboratory for further processing.
Sperm Collection and Preparation
On the day of egg retrieval, the male partner or sperm donor provides a semen sample. If necessary, sperm can also be obtained through other methods, such as testicular aspiration or surgical extraction. The sperm sample is then processed in the laboratory to separate the highly motile and healthy sperm from the seminal fluid.
Fertilization
In the laboratory, the eggs and prepared sperm are brought together for fertilization. There are two main methods of fertilization used in IVF:
- Conventional IVF: In this method, the retrieved eggs and prepared sperm are placed together in a culture dish and allowed to fertilize naturally.
- Intracytoplasmic Sperm Injection (ICSI): ICSI is used when there are concerns about sperm quality or when previous IVF attempts have not resulted in successful fertilization. In ICSI, a single sperm is selected and injected directly into the egg using a fine microneedle.
Embryo Development and Monitoring
After fertilization, the eggs develop into embryos under carefully controlled laboratory conditions. The embryos are monitored for several days to assess their quality and development.
Embryos may be graded based on factors such as the number of cells, symmetry, and fragmentation. The best-quality embryos are selected for transfer, while others may be cryopreserved (frozen) for future use. An embryo biopsy can also be done at this time for preimplantation genetic testing (PGT).
Embryo Transfer
Embryo transfer is placing the selected embryos into the woman’s uterus. The procedure is usually performed 3-5 days after egg retrieval or, in some cases, after the embryos have been cryopreserved and thawed.
A thin catheter is used to transfer the embryos into the uterus through the cervix carefully. The number of embryos transferred depends on various factors, including the woman’s age, embryo quality, and previous IVF outcomes.
Embryo Implantation and Pregnancy
Following the embryo transfer, the woman is typically advised to resume normal activities.
If successful, the transferred embryos implant into the uterine lining, leading to pregnancy. Approximately 10-14 days after the transfer, a pregnancy test is conducted to determine if implantation has occurred.
Challenges and Success Rates
 In the United States, the national average for women younger than 35 who become pregnant by in-vitro fertilization (IVF) on the first try is 55%, but this also depends on whether eggs are frozen or freshly retrieved.
In the United States, the national average for women younger than 35 who become pregnant by in-vitro fertilization (IVF) on the first try is 55%, but this also depends on whether eggs are frozen or freshly retrieved.
While IVF has provided hope to many couples struggling with infertility, it is essential to acknowledge that it is not a guaranteed solution, and success rates can vary depending on several factors.
Some challenges and considerations associated with IVF include:
- Age: The woman’s age is a significant factor that affects IVF success rates. Generally, younger women have higher success rates due to better egg quality and ovarian reserve.
- Ovarian Response: The response to ovarian stimulation can vary among individuals. Some women may produce a lower number of eggs, while others may experience ovarian hyperstimulation syndrome (OHSS), a condition characterized by enlarged ovaries and fluid accumulation.
- Embryo Quality: The quality of embryos plays a crucial role in the success of IVF. Not all embryos have the same potential for implantation and development; therefore, selecting the best-quality embryos for transfer is important.
- Multiple Pregnancies: IVF carries a higher risk of multiple pregnancies, particularly if more than one embryo is transferred. Multiple pregnancies are associated with increased health risks for both the mother and the babies.
- Emotional and Financial Considerations: Treatment costs, medications, and additional procedures can increase quickly. It’s a good idea to sit down, evaluate your budget, and explore financial options such as insurance coverage, flexible spending accounts, or payment plans offered by fertility clinics such as The IVF Center’s. Some could also explore fundraising or grants to assist with fertility treatment expenses. You can effectively navigate IVF’s emotional and financial aspects with proper support and careful financial planning.
Success rates can vary depending on individual circumstances, including age, fertility diagnosis, and previous IVF attempts. On average, the success rates for IVF range from 40% to 50% per cycle for women under 35, gradually decreasing with age.