- What should you know about endometriosis?
- What is it like to have endometriosis?
- Is it hard to diagnose endometriosis?
- Can I get pregnant if I have endometriosis?
- Is endometriosis treatable?
March is Endometriosis Awareness Month, a time we focus on raising awareness for this painful and debilitating condition that causes tissue that normally grows within the uterus to grow outside it in the pelvic region of the body.
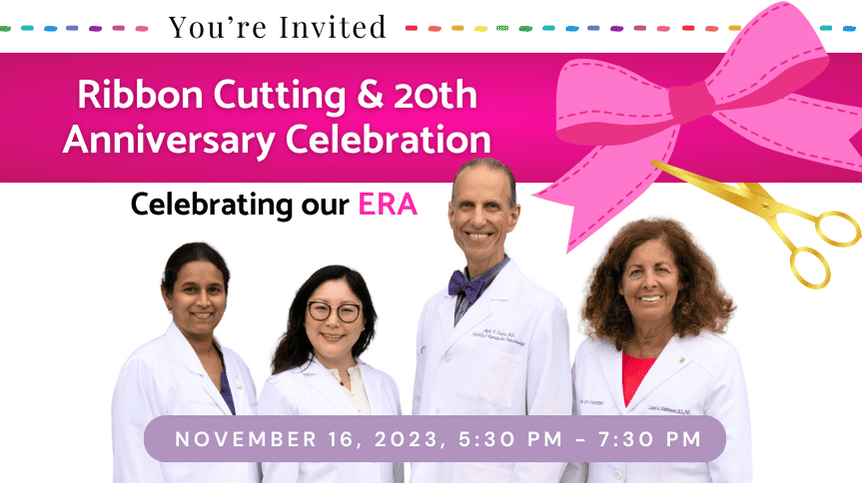
Dr. Mark Trolice, FACOG, FACS, FACE, board-certified reproductive endocrinology and infertility specialist at The IVF CenterSM, knows firsthand the difficulties inherent in diagnosing and treating this illness. He says, “Endometriosis is considered ‘the great masquerader’ because it mimics so many other disease processes.”
What Should You Know About Endometriosis?
Simply, endometriosis is normal tissue lining the uterus (endometrium) located anywhere else in the body. Typically, endometrial tissue (endometriosis) shows up in the on the ovaries but can also be found on the fallopian tubes, anywhere in the pelvis. In fact, endometriosis has been found in every part of the body except the spleen.
In a normal menstrual cycle, the lining of the uterus changes – immediately following the shedding of the uterine lining with menses, the endometrium begins to build and grow thicker until ovulation then is stable for the two weeks following ovulation until menses recurs (unless there is a pregnancy). With endometriosis, the endometrial tissue outside the uterus can go through this same process. Instead of bleeding out as part of the menstrual cycle, the tissue outside the uterus has nowhere to slough off. This tissue can become trapped in the pelvis, grow irritated, develop scar tissue, and even cause the organs to stick together.
Endometriosis affects 10-15% of all women and more so in the infertility population. Of women with endometriosis, 30-50% are estimated to have infertility. While 20-50% of women with infertility are found to have endometriosis. During surgery, endometriosis can be graded into stages – 1 to 4 based on severity. Low stage disease has a weak association with infertility but more advanced cases has been shown to reduce fertility. Surgery may improve fertility when women have advanced stage disease. Following surgery, recurrent rate is estimated to be 19% after two years and 40-50% after five years.
What is it Like to Have Endometriosis?
For those with endometriosis, the chief symptom is pain. This could include:
- Extremely painful menstrual cramps that seem to get worse over time
- Chronic aching pain in the pelvis and lower back
- Painful sex either during or afterwards
- Intestinal cramping and pain
- Painful urination during a period and/or bowel movements
There may also be bleeding or spotting between the menstrual periods or digestive problems such as nausea, diarrhea, constipation, and bloating. These symptoms mirror many other types of illnesses, making endometriosis extremely hard to diagnose. Since one of the long-term effects of endometriosis is infertility, this can be a serious problem.
Is It Hard to Diagnose Endometriosis?
It is very difficult to determine whether endometriosis is the cause of reported symptoms. Dr. Trolice says, “It has been reported to take 6 to 11 years for an endometriosis diagnosis. The delay is especially seen in adolescents who may not stress their level of pain since they are new to menstruation.”
Sometimes endometriosis can be misdiagnosed as other painful pelvic conditions. This could include:
- Fibroids
- Ovarian cysts
- Pelvic inflammatory disease (PID)
Endometriosis is often mistaken for appendicitis, because right sided lower abdominal pain can be a characteristic of both illnesses. Urinary tract infections cause painful sex and pain upon urination—which are also symptoms of endometriosis. Even sciatica, which causes pain in the back, legs, and buttocks, can mimic the back pain from endometriosis.
Endometriosis sometimes causes diarrhea, abdominal cramping, and constipation. This makes the illness resemble irritable bowel syndrome (IBS). Ironically, IBS can sometimes be a co-diagnosis with endometriosis, so treatment for both conditions may be needed.
The U.S. Department of Health & Human Services Office on Women’s Health shares the research showing that endometriosis is linked to several other types of illness, including:
- Allergies and asthma
- Autoimmune diseases like lupus, hypothyroidism, or multiple sclerosis
- Chronic fatigue syndrome and fibromyalgia
- Ovarian and breast cancer
Once endometriosis is finally diagnosed, one of the biggest questions asked by is whether pregnancy is still possible.
Can I Get Pregnant If I Have Endometriosis?
Yes, getting pregnant when suffering from endometriosis is possible. The disease may make it harder to get pregnant, but depending on age and physical condition, pregnancy is still likely. Approximately 70% of those who have mild or moderate endometriosis often get pregnant without fertility treatment.
While we do not yet fully understand the link between endometriosis and infertility, the volume of endometrial tissue and its location seem to affect reproductive health and the ability to conceive.
The National Institute of Health (NIH) suggests some of the possible reasons endometriosis causes fertility issues is:
- Patches of the endometrial lining change the shape of or somehow block the reproductive organs, and pelvis
- The endometrium, or the uterine lining where embryo implantation occurs, doesn’t develop properly
Is Endometriosis Treatable?
Medications and surgery are available to treat endometriosis. When seeing a doctor, there will likely be several tests to confirm the diagnosis of endometriosis. This could include:
- A complete examination and history
- A pelvic exam where the doctor palpates the abdomen and pelvis
- An ultrasound to help the doctor see your reproductive organs and the surrounding tissue inside the body
- Possibly, an MRI, or magnetic resonance imaging test, which uses radio waves and magnets to get a better picture of inside the body
- Laparoscopy surgery may be necessary, so the doctor can use a tiny camera to look inside the body and take a biopsy tissue sample
The treatment for endometriosis is usually medications or surgery, but it depends on whether a mild, moderate, or severe case of the disease has been diagnosed. For moderate cases, over-the-counter treatments such as NSAIDs, ibuprofen, or naproxen sodium, as well as heating pads on the abdomen could alleviate symptoms.
If these treatments don’t work, a doctor may consider prescribing:
- Hormone contraceptives such as birth control pills
- Gonadotropin-releasing hormones (Gn-RH) to block the body’s estrogen which shrinks endometrial tissues
- Progestin therapies
- Aromatase inhibitors to reduce the amount of estrogen in the body
If all of these treatments fail, the doctor may discuss surgery as the next option.