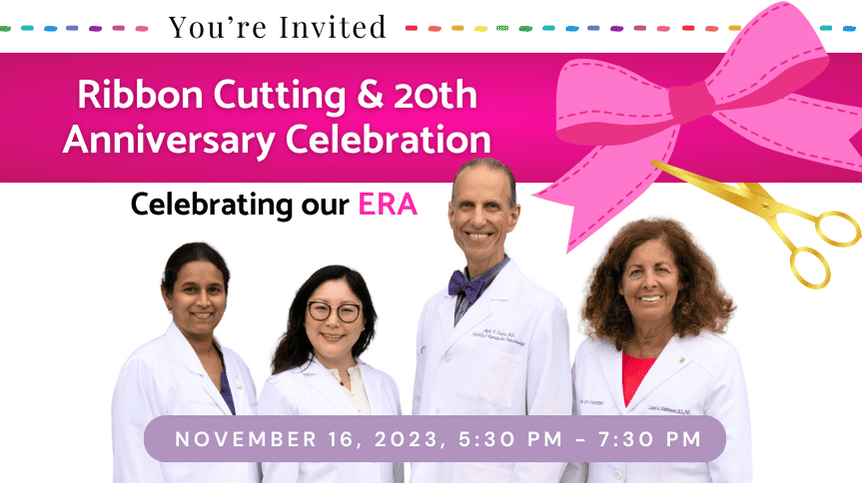
When a 47-year-old woman delivered an IVF baby a few years ago—it was a major accomplishment. With the declining U.S. birth rate and a growing number of women utilizing in-vitro fertilization (IVF), an important question is “what is the upper limit to pursue IVF as a viable option to have a baby?”
When a 47-year-old woman delivered an IVF baby a few years ago—it was a major accomplishment. With the declining U.S. birth rate and a growing number of women utilizing in-vitro fertilization (IVF), an important question is “what is the upper limit to pursue IVF as a viable option to have a baby?”
Realistically, you can always undergo IVF unless you have experienced ovarian failure and/or menopause. However, pregnancy success rates using your own eggs drops considerably for women over 40.
In the U.S., the likelihood of achieving a live birth from one egg retrieval in women between ages 41-42 is less than 20% (http://sart.org); in women above age 42, the rate is less than 5%. This coincides with the increasing percentage of chromosomally abnormal embryos tested by PGT-A (preimplantation genetic testing)—which rises to over 80% abnormal in women above age 42.
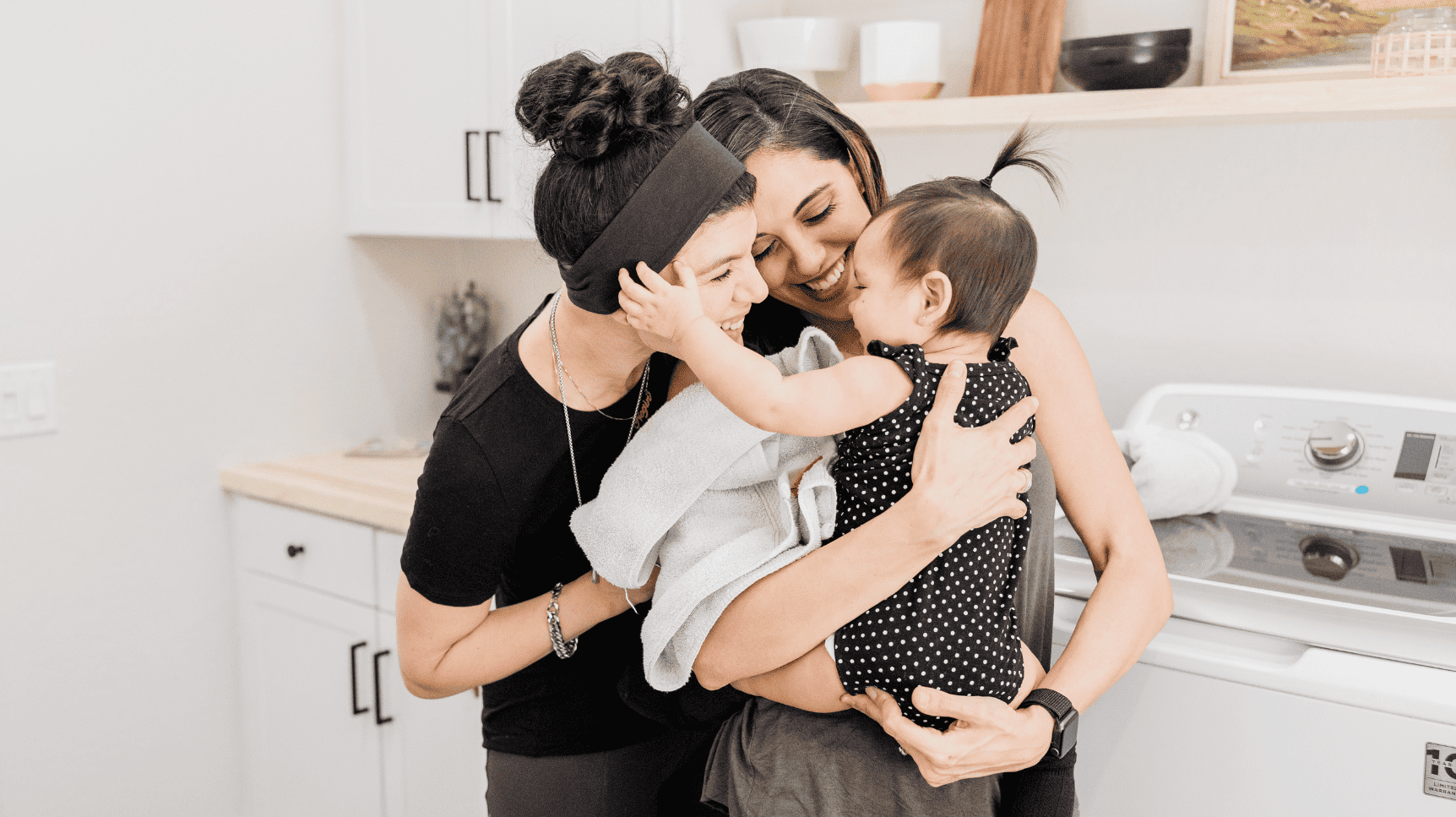
Am I Too Old to Have a Child? Meet Amanda
On a recent flight, I sat next to a professionally dressed woman (let’s call her Amanda), who was the owner of a very successful language translation company. She started the company immediately after college. Amanda was inspired from her father’s significant communication challenges on his business trips to foreign-language countries. When I shared my profession, she responded with a deep disappointing sigh. It wasn’t that Amanda didn’t like my field of medicine. She had never had children, and now she was 45.
Amanda’s reproductive life choice became the new focus of our chat. She was a driven entrepreneur who experienced multiple “forks in the road” during her professional career. Rather than having children as a single mom, she chose to wait for a relationship that never occurred. Then came her million-dollar question to me, “Am I too old to have a child?”
The question is simple enough. The answer, unfortunately, is extremely complex. Amanda, like many women, delayed childbearing due to the lack of a partner and/or for career reasons. The result of the shift in parenting plans is this startling statistic – a 30-year low in U.S. birth rates over the last 10 years and the average age of first-time mothers advances globally. In 2017, women in their 40s were the only group with a higher birth rate. Women above age 35 also showed an increase in first-time births.
What is Diminished Ovarian Reserve?
Let’s start by understanding the concept of diminished ovarian reserve (DOR), or ovarian aging. Women are born with all the eggs they will use in their reproductive lifetime (1-2 million at birth reduced to 200,000 to 400,000 at puberty), resulting in approximately 450 ovulations per lifetime. Monthly, hundreds of eggs vie to ovulate, but only one is successful while the rest get reabsorbed into the body. This cycle continues until menopause.
DOR is currently best measured by considering your chronological age, antral follicle count (AFC) by pelvic ultrasound and by a blood test for anti-mullerian hormone (AMH) blood test. Although other factors contribute, the main determinant of pregnancy rates is egg quality.
The quality of eggs is based on your birthday – the more birthdays you have, the steady decline in fertility, beginning around age 30, due to egg quality diminishing. Quantity, on the other hand, is indirectly determined by AMH and AFC. AMH levels below 1.6 ng/mL have been shown to reduce the number of eggs retrieved following ovarian stimulation as part of IVF. Levels below 0.4 are severe and seriously reduce IVF success rates. AFC uses vaginal ultrasound to counts the number of small cysts (antral follicles) in the ovaries. Less than 11 AFC reflects the beginning of DOR, while less than 6 is severe.
What does ovarian age testing NOT help with?
It is wise to use some caution with DOR test results. The use of a screening test for DOR in a population at low risk for infertility (meaning women under 35 years of age) will result in some women experiencing unnecessary alarm. The reason? Ovarian age testing does NOT predict your natural fertility or the age of menopause.
A recent medical study did not show a difference in natural pregnancy rates in women aged 30-44, irrespective of AMH levels. While the results of AMH screening may make you think “freeze my eggs,” there is no reliable evidence that AMH levels should be used to decide on egg freezing or to avoid IVF.
 Should You Use an Egg Donor?
Should You Use an Egg Donor?
If we compare the disappointing pregnancy rates for women in their 40s who use their own eggs to success rates using egg donation, we see the latter group having a much higher success rate – nationally nearly a 50% live birth rate.
The decision to use an egg donor is a significant emotional challenge. The choice is made even more confusing given the media display of celebrities in their late 40s and early 50s not disclosing, but presumably, having used an egg donor. This lack of transparency only heightens your stress and creates unrealistic expectations when you are faced with DOR.
Amanda’s Decision
By the end of the flight, Amanda began to realize that the journey does not equal the destination. She asked for the names of fertility specialists in her area that can offer egg donation. Her expedited and calculated decision left no doubts as to why she attained her position in business.