 The focus of infertility treatment traditionally has primarily been on the female. However, in almost 50% of couples, the male is in fact responsible for infertility. Recent research has shown that males now produce less than half as many sperm than males in the early 1970s. In addition to having lower quantities, sperm are now are also of lower quality.
The focus of infertility treatment traditionally has primarily been on the female. However, in almost 50% of couples, the male is in fact responsible for infertility. Recent research has shown that males now produce less than half as many sperm than males in the early 1970s. In addition to having lower quantities, sperm are now are also of lower quality.
So, how can men improve their fertility?
In this episode, Jamin Brahmbhatt, M.D., a board-certified urologist specializing in chronic testicular pain and infertility, joins host Mark P. Trolice, M.D., to discuss the male role in infertility and what men can do to protect and preserve their fertility. Listen in as he shares insights on everything from low sperm count treatment, sperm freezing, and hormone treatment to diet, marijuana use, and alcohol consumption.
Tune in to discover:
- What lifestyle changes men can do to protect their fertility and stay healthy
- How mental health can affect a man’s fertility
- The impact of age on male infertility
- What to expect when visiting a urologist for an infertility consultation
- The types of interventions available for men to improve their fertility
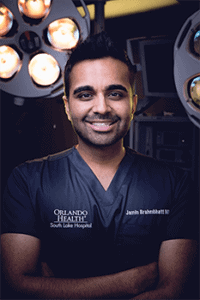 About Jamin Brahmbhatt, M.D.
About Jamin Brahmbhatt, M.D.
Dr. Jamin Brahmbhatt is a board-certified urologist specializing in chronic testicular pain and infertility. He completed his urology residency at the University of Tennessee followed by a fellowship in robotic microsurgery at the University of Florida. He is now co-director of PUR Clinic (Personalized Urology & Robotics) at South Lake Hospital & Orlando Health.
He is an active member of several professional organizations including the American Urological Association, SMSNA, CAPI, and the Florida Urological Society where serves on the executive committee. He is a TEDx speaker and winner of numerous awards including 40 under 40 and Top Doctor.
He is frequently seen offering expert medical opinions on national media platforms and his own social media channels. He is the co-founder of the Drive 4 Men’s Health, an annual non-profit public engagement campaign that continues to encourage millions of men to eat better, get active, and engage in preventative medical screenings.
About Mark P. Trolice, M.D.
Mark P. Trolice, M.D., FACOG, FACS, FACE is Director of Fertility CARE: The IVF Center in Winter Park, Florida and Associate Professor of Obstetrics & Gynecology (OB/GYN) at the University of Central Florida College of Medicine in Orlando responsible for the medical education of OB/GYN residents and medical students as well as Medical Endocrinology fellows. He is past President of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past Division Director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double Board-certified in REI and OB/GYN, maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a Fellow in all three American Colleges of OB/GYN, of Surgeons, and of Endocrinology. His colleagues select him as Top Doctor in America® annually, one among the top 5% of doctors in the U.S. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For ten years his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology as well as the editorial advisory board of Ob.Gyn.News. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines and newspapers on reproductive health topics. His current book is on the Infertility journey to be published by Harvard Common Press in mid-2019.
Transcription Notes
Speaker 1: Thanks for tuning in to The Fertility Health Podcast hosted by renowned fertility specialist Mark Trolice MD. Each episode features firsthand advice and potential treatment news, tips, and strategies listeners can use on their fertility journey. Now here is your host, Dr. Trolice.
Mark Trolice: Hi, everyone. Welcome to the Fertility Health Podcast. I am your host, Dr. Mark Trolice. Joining me today to discuss evaluating the male in the fertility pursuit by men or couples is a good friend, Dr. Jamin Brahmbhatt. Dr. Brahmbhatt is a board certified urologist specializing in chronic testicular pain and infertility right here in central Florida.
Mark Trolice: He completed his urology residency at the University of Tennessee followed by a fellowship in robotic micro surgery at the University of Florida. He is now co-director of the PUR Clinic and PUR stands for Personalized Urology and Robotics at South Lake Hospital and Orlando Health, as I said, in central Florida.
Mark Trolice: He’s an active member of several professional organizations including the American Urologic Association and the Florida Urologic Society where he serves on the executive committee. He’s a TED speaker, he’s on the media in every area of television and radio and print. He’s frequently seen on national platforms as well as social media channels.
Mark Trolice: I don’t know if you’ve seen him and his associate Dr. Sijo Parekattil. They’ve co-founded this Drive For Men’s Health. It’s an annual nonprofit public engagement campaign that continues to encourage millions of men to eat better, get active, engage in preventive medical screenings. I enjoy following his career not just in the medicine but what he does outside of medicine to pursue a better male health.
Mark Trolice: This is going to be on the infertility evaluation, which is not excluding the health of the male because there are lifestyles and behavior modifications, which I hope he gets into to talk about how the men can improve their fertility just by doing those things.
Mark Trolice: You know, the male aspect of fertility, which most people are not aware of, is that 40% of couples it’s the male that has a problem that’s contributing to fertility. It’s almost half.
Mark Trolice: Let’s get into it. We bring in, Dr. Jamin Brahmbhatt. Jamin, thank you so much for joining The Fertility Health Podcast and for taking the time today.
Jamin B.: Hey, Dr. Trolice. Thank you for having me on this podcast. I think this is a very good topic to bring up because to be very honest with you when patients show up in my office before they show up in my office they kind of assume that 100% of the cause of their infertility issues are because of the female but the reality is that around 50% can be male-related. It’s a team effort in working with the female, working with the male, and getting the couple what they want, which in this case would be parenthood.
Mark Trolice: Yeah. Absolutely. I even see that in some reproductive clinics where the male is not even evaluated. They feel that you could just go right to IVF and sort of overcome that, which is obviously not the right thing to do. Our listeners need to know that an abnormal sperm analysis might be the first sign of something really even serious like God forbid cancer. You always want to evaluate the male not just for the fertility reasons but for health.
Mark Trolice: To talk about the outset, Jamin, what lifestyle changes can a man do to protect his fertility but also if he’s having trouble what are some things that they want to avoid?
Jamin B.: The testicles are a very sensitive organ. They like to be in a certain place, certain position, certain temperature and have a lot of things around them balancing the chemicals and the hormones around it. One of the biggest risk factors for infertility is our obesity epidemic. Not only is obesity causing high blood pressure, diabetes, strokes, and many other problems but it’s also linked with a dysfunction within the testicle itself when it comes to being able to produce good, amazing, awesome sperm.
Jamin B.: Not only that but anything that changes location or temperature around your testicles, which could include sitting in hot tubs all day, laptops, the whole theory about boxers versus briefs, to be very honest with you there was no direct link so enjoy whatever you like to wear, but hot tubs and laptops which can really increase the heat around the testicles is directly correlated with issues with infertility.
Jamin B.: One of the biggest things a lot of people don’t talk about is actually mental health, stress. Most of us Americans are stressed either at work or at home. Stress is directly related to how well your testicles are going to be able to produce that optimal sperm.
Jamin B.: If you’re stressed out, obese, and taking part in things like smoking or supplementation or bad habits, all of that stuff is not only going to cause you to have issues with fertility today but all of those things are also linked, as you mentioned already, with other health issues in the future. There’s no better time than now to get that wake-up call and start improving these things.
Mark Trolice: Yeah. Tobacco, a big problem of course, and it seems like there’s some effects on genetic alterations of the sperm. It’s not just the female, which we really, really encourage our women to stop because of the accelerations in ovarian aging with cigarette smoking but tobacco is still a big problem.
Mark Trolice: What other things are you seeing that men need to avoid? I know the endocrine disruptors, the [inaudible 00:06:16], these chemicals, the plastics, all of those things seem to have some impact on sperm as well.
Jamin B.: Yeah. Well, I just want to finish [inaudible] cigarette smoking. Vaping is becoming huge right now, especially in kids that are teenagers, middle school kids. We don’t know the exact links yet but I bet you we can safely assume that it’s going to cause the same issues that smoking does when it comes not only to its carcinogenic effects but it’s effect on fertility.
Jamin B.: Don’t forget that aspect. Like, “Oh, I just vape so it’s okay for me to continue while I’m having these issues.” No, not only that but marijuana as well. I’ve probably seen like three patients this year that just stopped their marijuana use for a couple months and everything went back to normal without any medications, without any manipulation, or any surgical intervention.
Jamin B.: Anything that you’re not supposed to be putting in your mouth or smoking is directly going to affect your fertility. You should really be cognizant of all that stuff today rather than worry about it tomorrow.
Mark Trolice: Yeah. There was an article today talking about the harmful effects of marijuana. I think we’re going to be getting a lot more data now that there’s a medical marijuana push across the country. We’ll be able to get more studies I’m sure to see the true effects of marijuana on fertility as well as other things.
Mark Trolice: I also see that a lot of the men are extremely surprised over the age factor. For many years we thought it was really women’s reproductive age had that cut-off and that men could be able to father a child well into their later years. Now we’re seeing age having an effect on reducing fertility and increasing miscarriage, birth defects, and even some autism and schizophrenia particularly in the men above 40 to 45 increasing fourfold.
Mark Trolice: What are you telling the men at a younger age? Are you giving them a heads up to say that, “Hey, this is not something that is lifelong fertility. There is a biologic clock for men”?
Jamin B.: It’s not as straightforward for me because, yes, there’s all this data out there but it’s not as strong as it is for you in your field. I always tell patients, “You’re not going to be any healthier five or 10 years from now than you are today.”
Jamin B.: What we do know is that men do have a natural decline in testosterone after the age of 40 so that being said there’s probably a natural decline in other things in your testicle as well and that is sperm.
Jamin B.: Yes, men could have sperm up until 100, up until the day they’re dying, but how efficient are those sperm going to be? It’s kind of like you can climb Mount Everest today but 20 years from now it’s going to become much harder. That’s the same thing when it comes to your [inaudible] fertility. It’s going to be harder for you but it may also be harder for the baby and its future.
Jamin B.: A lot of patients are waiting nowadays and there’s actually a big push in some of these big cities for guys that are going to plan on waiting to go ahead and freeze their sperm, which sounds like a great idea but is it really worth freezing and delaying a natural process? I think that’s a debate for another day.
Mark Trolice: Yeah. I did not know. People ask me, “Are men doing that?” Are you starting to hear about that across the country?
Jamin B.: I have colleagues of mine in New York City that get a lot of these Wall Street guys that just go ahead and bank some sperm.
Mark Trolice: Like the women are doing with egg freezing. Interesting. Let’s start from an exam. You get referred a male with an abnormal sperm analysis. Talk us through how you would evaluate these men from the beginning. Obviously the history and examination and so on.
Jamin B.: When the men come to my office I always request that if their partner can come with them or we can get them on the phone or on Facetime at the same time so that way we’re clear on exactly what we’re going to be doing and also we can clear up some of the statistics. There’s a lot of guilt involved with some of this stuff as well because one sex may be blaming the other sex.
Jamin B.: The evaluation, as you mentioned, starts off with a semen analysis. That’s where you would basically go and masturbate for us in a cup and then we would analyze your sperm. Now that has to be done two times because there’s so many things that you could be doing today that could affect your sperm counts tomorrow. We always want to get a good two data sets when we assume, “Okay, there’s definitely something wrong.”
Jamin B.: On top of that what we’ll do is we’ll get some lab work. Your testicle is driven by signals from your head, from your brain. Those chemicals have to interact with your testicles and then once your testicle makes sperm it travels through these small little tubes and joins your prostate in the ejaculatory ducts and then your sperm is actually a very small part of your ejaculate. All that stuff that you see that comes out only about 10%, 15% is actually sperm.
Jamin B.: There’s a lot of processes where things go wrong so that’s why we check several different things and that includes the semen analysis, it includes lab work to look at your entire hormone profile, and then it also includes an examination where I’m actually feeling the testicle, feeling those tubes, and seeing if there’s any deformities, abnormalities, or absences of these few things that I may be used to seeing on a normal patient.
Jamin B.: Based on what we find on that then it may lead into more testing, it may lead into further imaging like ultrasounds, it may lead into very invasive testing like genetic testing, or it may be a recommendation to either move forward with surgery with us or we may say, “Hey, you know what? If you want to pursue other options then maybe something like IVF may be the best way to go” because we not only take into account the male. We take into account the female and all of her risk factors as well when we’re having these discussions with our couples.
Mark Trolice: You know, our literature is such that we will refer after one abnormal sperm analysis. Are we jumping the gun? Should we wait for these men? Should you see them and do the second sperm analysis?
Jamin B.: I would say the best is to have two. When you guys do send us these patients … The ideal patient that would come in at least for me would have two semen analyses and the full hormone profile done. It’s really just for the patient’s convenience because when they have all that stuff done they see me in the office and then we can start with a treatment or start taking more aggressive steps.
Jamin B.: When I get patients with just one semen analysis it’s okay. I don’t mind. Then we would just order everything and then I would just see him a couple weeks later. We’re saving some time but we’re not saving them from expediting anything else that they would need done.
Mark Trolice: I often get a little bit stymied over men who have just the isolated low shapes and/or just low volume. Everything else being normal. What do you do with just isolated low volume? What do you do with just isolated low shapes?
Jamin B.: Yeah. When it comes to low volume that’s why we always get two. A lot of these patients don’t refrain for two or three days before they actually ejaculate. Some of them may admit that they actually missed the cup when they were doing it in the office. That’s why we like to get two.
Jamin B.: Now when you say low volume it really depends on the number that we get. If it’s super duper low then we may pursue some genetic testing and further imaging because there may be something anatomic or something on a microscopic level in the testicle that could be causing these low numbers.
Jamin B.: If it’s just borderline there’s millions of couples out there getting pregnant on borderline sperm counts. There’s actually millions of couples out there getting pregnant with very few sperm counts. You can’t just always go by the counts.
Jamin B.: Now you mentioned morphology or the shape. I don’t really put too much into morphology. I think it may really affect things when it comes to them doing IVF but for me the two biggest things I look at is the count and I look at the mobility. Like how well are they really moving?
Jamin B.: These are two things that I can really improve either with some surgical interventions or medications or, to be very honest with you, behavior changes. Like some of these guys I’ll just say, “Hey, you’ve got to lose some weight, you’ve got to stop smoking, and then let’s recheck everything in three months.”
Jamin B.: Mark, I mentioned three months and that’s a very important time period to remember. Three months is the life cycle of sperm. If you were to change and make some major life changes today we honestly probably won’t see many changes until about three months into the actual semen analyses. A lot of this stuff is not instantaneous. It takes some time.
Jamin B.: That’s why you’ve got to take into account the whole picture when you’re recommending some of these interventions because some patients may not have time to wait.
Mark Trolice: Right. Right. Exactly. A good point that you were talking about in terms of the parameters of the density and mobility, the count and the motions of the sperm, I think it’s important for our listeners to know that the World Health Organization has given us guidelines for what we consider normal and not normal for sperm analyses.
Mark Trolice: A little bit of background. The way that they came up with these guidelines, which was back in 2010, actually they released the fifth edition, is that say you take 100 fertile men, they’re all fertile, meaning that they impregnated a woman within a year of trying, and they looked at the 95% cut-off.
Mark Trolice: All the men were able to impregnate and so the men that are outside those parameters, lower than those parameters, could still be fertile but there’s just less of them. There’s like 5% of them essentially. I think that a lot of people get the misunderstanding, Jamin, that if the numbers are below those cut-offs that, “Oh my gosh. There’s no way we’re going to be able to conceive naturally.”
Jamin B.: No, because you need to think of it like a graph. You’ve got the 5% on one extreme and the 5% on the other extreme. I mean, I see men with 300 million sperm, which for our listeners that’s a lot of sperm. I call them supermen. They may still have issues with fertility.
Jamin B.: That’s because there’s a sub-segment of these patients that have unexplained infertility. The female may have a perfect work-up, the male may have a perfect work-up, but there’s still some issues on a microscopic level, which we just don’t have the best understanding of where they’re not able to conceive.
Jamin B.: That’s when we really after we’ve tried on both of our ends may start recommending, “Hey, maybe it’s really time to get aggressive and do something like IVF or IUI if you haven’t done it.” There’s certain parts where we just can’t explain why they’re not interacting in there and that’s the unexplained infertility part.
Mark Trolice: Yeah. You get into the circumstances where … I remember when I was in Charlotte. A young couple, everything normal, tubes are open and she ovulates, and his sperm analysis was normal, they went through multiple, multiple IUI cycles. We do IVF. No fertilization. That was the problem. The sperm were not able to bind to the egg to result in fertilization so we had to do the advanced technology of [inaudible] where you take a single sperm and inject it into the egg.
Mark Trolice: The sperm analysis … I’m hearing more and reading more that the sperm analysis is not really a very good test to determine reproductive potential of a man, correct?
Jamin B.: No, no. It’s not at all but unfortunately that’s all we have. It’s kind of like a snapshot of your day. We just use a tool. Some people get so obsessed with it. That’s why I don’t really focus on the nitty gritty details.
Jamin B.: You have to understand, the semen analysis as well there’s a lot of subjectivity to it as well. If it’s done somewhere where someone is looking … We don’t look at the whole all the CCs. They look at sub-segments of it. There’s a lot of variation sometimes. There’s all these new technologies where it’s computerized and it can be done but they’re still a variation.
Jamin B.: What we try to look for is trends. Based on the trends we make decisions, whether it’s medications to help boost their testosterone or block your estrogen receptors, which can help hopefully boost your count, or if there’s something anatomic like if you have had hernia surgery and now your tubes are blocked.
Jamin B.: That’s when we may not see any sperm come out then we can do a reconstruction or I see a lot of men, Mark, that are on testosterone injections and they go through all this stuff and then they finally admit, “I’m taking testosterone at the gym. I haven’t told my wife. Please don’t tell her.” Then we end up stopping it and things go back to normal or they may have something anatomic like [inaudible] which are being veins.
Jamin B.: There’s definitely things that we can correct but honestly a lot of the times if they focus on some of the behavior things early on in their life they can potentially avoid a lot of the pokes and prods in the future.
Mark Trolice: Yeah. You briefly touched on the [inaudible] Just for our listeners, I don’t know if you’re familiar … I guess an easy thing to say is the varicose veins in the legs, the veins are very prominent. Particularly in tall men on the left side of their scrotum they could have an increase of veins, which is what we call congestion, and it’s because of the way the vein drains into the rest of the body, the renal vein. It could cause a backflow of blood and that increased temperature can have an effect.
Mark Trolice: It seems that the evidence is such that if you can feel it and there is an infertility and abnormal sperm analyses those are the patients that would benefit from surgery, not if it’s visualized just by ultrasound or any other special imaging. Feeling it … It feels like a bag of worms around the testes.
Mark Trolice: What can we take home, Jamin, for our patients in terms of optimizing their fertility for men?
Jamin B.: You mentioned the varicose thing. You’re absolutely right. There’s three grades to it. Grades two and three have been shown to definitely benefit these patients.
Jamin B.: A lot of my men will not have [inaudible] There will just be some hormonal deficits. To kind of summarize what are the things that you can do today? Well, anything that keeps your heart healthy is going to keep your balls healthy and is going to help your fertility. Get your 150 minutes of moderate exercise in a week.
Jamin B.: You can be a weekend warrior, you can spread it out 30 minutes a day, but keep your heart pumping, keep your blood fresh, keep your oxygenation positive, and now that stuff is going to keep you from getting overweight and obese and that’s going to lead to a trickling down effect where you’re going to have improved fertility.
Jamin B.: The second thing is you are what you eat. The testicle is very sensitive. Make sure you have a very well-balanced diet. When I say well-balanced diet that does not include alcohol. Patients that are known to be excess alcohol drinkers … In men, I think that number is more than 10 drinks a week. Alcoholism is also linked with infertility as well.
Jamin B.: Get moving more, make sure you’re putting the right things in your mouth, and the third thing is if you do have a problem or you do have an issue don’t wait too long. Get it fixed now. Especially with fertility things. You may get this corrected now, you may have the baby now, but still keep following up because these same things are going to cause issues with testosterone in the future, which can affect your mood and your bones and your muscle mass and many other things. It’s kind of like an eye opener now that should require lifelong followup in the future.
Mark Trolice: Excellent points, Jamin. We’re running out of time unfortunately. I just wanted to underscore the point that testosterone is given out much too frequent for men in their reproductive years who are complaining of fatigue and their primary care physicians will give them that or if they’re doing bodybuilding.
Mark Trolice: Unfortunately, testosterone can suppress and block these signals from the brain and cause no sperm in the ejaculate. If it’s not too long that you’ve been on it hopefully stopping it will restore sperm but sometimes if you’ve been on it for a long time it may not be able to be restored and you have to get sperm from the testes.
Mark Trolice: We’ve run out of time. I could probably talk for another half hour or more with Dr. Brahmbhatt. He’s a plethora of information. I want to thank you all for listening to The Fertility Health Podcast.
Speaker 1: Thanks for listening to The Fertility Health Podcast. If there’s anything from today’s show you want to learn more about check out the IVF Center dot com for all the notes, links, and tips mentioned in this episode.
Speaker 1: If you’re not already subscribed to the show please press the subscribe button on your podcast player so you don’t miss a future episode. If you haven’t given us a review or rating on iTunes yet consider leaving a five star review to help us reach and educate even more individuals in need. Thanks again for listening and we’ll see you next episode.






