One of the most difficult decision to make for both IVF Specialists (and our patients) is picking the number of embryos to transfer to the womb. In this blog & video interview, Dr. Trolice explains the responsible way to go about making this choice.
One of the most difficult decision to make for both IVF Specialists (and our patients) is picking the number of embryos to transfer to the womb. In this blog & video interview, Dr. Trolice explains the responsible way to go about making this choice.
An IVF cycle is a complex series of events all with the sole purpose of helping a woman deliver one healthy baby. Beginning with the decision to pursue IVF, the woman and/or couple undergo pre-cycle testing including procedures and blood-work to
optimize the outcome of the cycle.
Process
While on injectable hormones to stimulate multiple egg development, the woman receives ultrasound monitoring of the follicles (follicular cysts with eggs) of her ovaries along with blood-work to measure hormone levels.
Once the follicles grow to appropriate size, the woman is injected with a maturation hormone followed by egg retrieval approximately 36 hours later. The eggs are removed from the ovaries through needle aspiration, sperm are added later the same day, then embryos develop usually up to five – six days.
Of all involved, one of the most anxiety-provoking aspects for the woman/couple is the decision on the number of embryos to transfer. The goal is to maximize a single healthy live birth and minimize multiple births.
Understanding Embryo Transfer Guidelines
The following FACT SHEET and GUIDE will help you understand the risks of a multiple baby pregnancy including miscarriage, low birth weight, birthing complications and birth defects.
Why Do I Need to Worry about a Multiple Pregnancy?
BOOKLET: Multiple Pregnancy & Birth
Fortunately, the American Society for Reproductive Medicine (ASRM) has offered guidelines for physicians on recommending the number of embryos to transfer.
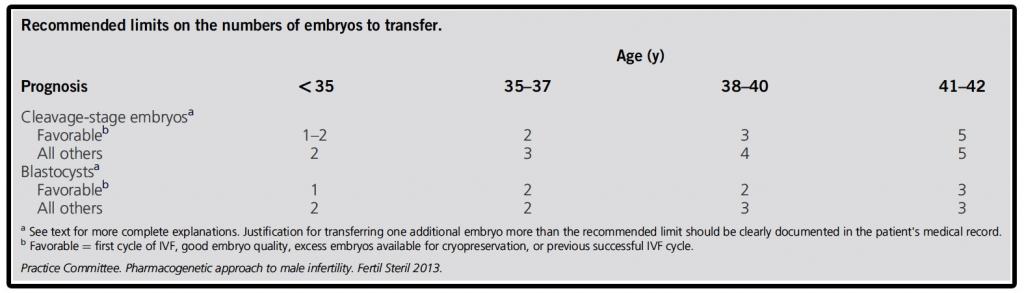
With more evidence demonstrating the advantage of a blastocyst (day 5 embryo) transfer, many IVF centers are encouraging patients to avoid cleavage stage (day 2 -3) embryo transfer, particularly in younger good prognosis patients. If all IVF cycles allow transfer on day 5, less than 10% of cycles would result in no embryos developing for transfer. An unanswerable question is whether an embryo that does not grow to day 5 would have resulted in a pregnancy had it been transferred on day 3?
Blastocyst transfer (BT) is more physiologic, meaning the embryo is placed intrauterine at the time occurring in a natural cycle. Further, BT allows for better selection of embryos for a single embryo transfer as well as the number of extra embryos available for freezing.
The following patient description is the optimal candidate for eSET:
- Younger than 35 years (35 – 40 is still an option with top quality Blastocyst Embryos)
- Undergoing their first assisted reproductive technology (ART) cycle
- Had a previously successful pregnancy using an ART cycle
- Has a relatively large number of high-quality embryos
- Has embryos available for cryopreservation (freezing to use in a later cycle)
ARTICLE FAST FACTS
- At the blastocyst stage, eSET pregnancy rate is equivalent to double embryo transfer (DET), but the latter has a much higher multiple pregnancy rate.
- Frozen embryo transfer number guidelines should be the same as fresh embryo transfer.
- Cumulative pregnancy rates of fresh and frozen cycles are the same with eSET vs. DET.